Indications
Wrist joint injection is a useful diagnostic and therapeutic procedure for inflammation due to rheumatoid arthritis and other inflammatory arthritides.
Techniques
After informed consent is obtained, the patient is placed in the sitting position with the arm resting on the examination table. The hand is placed palm down with the wrist positioned over a rolled towel. The wrist joint is approached from the dorsal aspect. The patient is prepared in a standard aseptic fashion over an area large enough to allow palpation of landmarks, and sterile technique is used throughout the procedure. A 1½-in. (4-cm), 23-gauge needle is inserted between the distal radius and ulna on the ulnar side of the extensor pollicis longus tendon. The needle is gently manipulated into the joint cavity to a depth of about 1 to 2 cm. Aspiration is attempted until the needle has entered the synovial space. If there is an effusion of the joint, the aspiration is completed. After negative aspiration or if the aspirated fluid is noninflammatory (clear and viscous), the joint is injected with a 2- to 3-mL mixture of 10 mg of triamcinolone acetonide (or equivalent) and local anesthetic (Fig. 67-43).
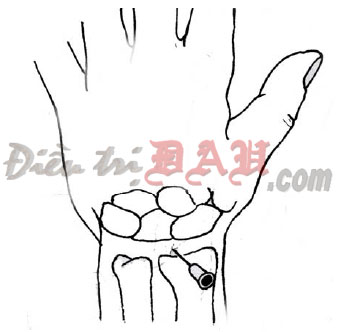
FIGURE 67-43. Wrist joint injection. Approach for wrist joint aspiration and injection.
Comments
Many of the synovial joints of the wrists are interconnected. No significant resistance should be encountered. If resistance is encountered, the needle may not be in the joint cavity. Scapholunate dislocation, carpal instability, avascular necrosis, or other etiology of chronic conditions should be considered before injection. Elastic bandage or splint immobilization for 24 hours after injection may decrease discomfort.
Complications
Intraneural injection may result in nerve damage. Hematoma and intravascular injection are possible due to the close proximity of the vessels. If an arterial puncture occurs, prolonged direct pressure is usually adequate to prevent the development of a hematoma. Corticosteroids should not be injected if there is any suspicion that the joint is infected. If the fluid appears infected, then it should be sent for culture and sensitivity and the patient treated appropriately for the infection.
Source: Physical Medicine and Rehabilitation – Principles and Practice
Originally posted 2014-03-17 13:55:47.

